Dr. Geoffrey Young on HPV-Related Head & Neck Cancer and RRP: Insights, Innovations, and Misconceptions

Background & Expertise
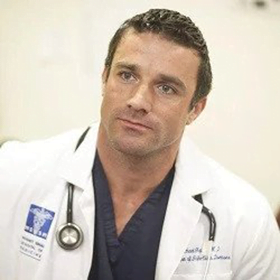
- Can you share a bit about your journey in medicine and what led you to specialize in head and neck cancer surgery?
Dr. Geoffrey D. Young, M.D., Ph.D., FACS, is the Chief of Head and Neck Cancer Surgery at Miami Cancer Institute and an expert in treating head and neck cancers, including those affecting the mouth, throat, larynx, thyroid, and salivary glands. During his training, he “discovered a passion for the procedural aspects of medicine” and “developed an appreciation for the anatomy of the ear, nose, and throat.” He began his career at the Mayo Clinic before being recruited to build a head and neck oncology program in Miami. Now involved with Florida International University (FIU), Dr. Young continues to advance patient care through innovative techniques like transoral robotic and laser microsurgery, ensuring comprehensive, multidisciplinary treatment for individuals facing HPV-related cancers.
- How has the landscape of HPV-related head and neck cancers evolved in recent years?
“If you look at the studies and the epidemiology we’ve seen an exponential increase in this disease in the last couple decades; and these trends seem to continue to be increasing.
“We will be having vaccinated individuals coming into play in data as well” Dr. Young mentions that this may take a few decades, but we may be seeing the same results as we’ve seen in cervical cancer reduction due to effective vaccinations in the future. Overall, the landscape of oropharyngeal cancer is seeing quite an increase in cases.
- Why is a multidisciplinary approach so crucial in treating HPV-related cancers, and how do you facilitate this collaboration?
“I feel that this is one of the diseases where a multidisciplinary approach is essential. The good news is that we know this disease (oropharyngeal cancer) responds well to treatment – However, there are many different options: surgical options, radiation-based options, and there are some patients that may need multimodality therapy. There are also clinical trials, because there’s a lot of research going on to the extent to which we treat the disease. So, given all of those factors, I think it’s very important that patients be evaluated in a multidisciplinary fashion with input from all of those specialties for the decision-making process.
Once you’re undergoing treatment, I think it’s also important to have the involvement of speech-language pathology, nutrition, and others to help people get through treatment. There’s the expression “It takes a village”, and with this disease it really does take a village because of the toxicities and changing landscape of treatment that we’re constantly adjusting to.
Having a patient centered approach is also very important because some patients are a perfect candidate for surgery but they are afraid, so they decide to go with radiation. Sometimes it can be either/or. You can have a patient who would like to avoid radiation so we have to push the surgical envelope a little bit to prioritize patients desires, comorbidities, or other precipitating factors.”
- Can you speak about any advancements in surgical techniques or treatment approaches for HPV-related head and neck cancers?
“Although it’s been around for a long time, 15 years or so, and in the surgical world that’s a long time …the biggest advancement really is transoral robotic surgery …. (this surgery) changed the landscape in being able to surgically treat patients with acceptable outcomes. Acceptable swallowing outcomes, acceptable co-morbidity outcomes, and plan to stay in the hospital for 1 day, maybe 2, it can prevent the need for radiation and or chemotherapy if the right criteria are met.”
Dr. Young goes on to note there are more advancements in the works – specifically “better ways to measure margins at the time of surgery, Fluorescent markers to help guide surgery to ensure adequate margins. All these things perpetuate and advance oncologic surgery.”
Surgical robots started off “fairly basic, using a robot that was designed for abdominal surgery, and now we’re starting to get more specialized robots with specific indications for transoral surgery.”
- What do you think is the biggest misconception about HPV-related cancers, particularly those in the head and neck?
This is a “two-part answer” Dr. Young states:
1) “There is a blame or guilt association that is not necessary – patients will say to me: did I or someone else in my life do something wrong for me to get this disease?.” Dr. Young specifies it is important to demystify this virus (HPV) for the patients self-assurance and comfort as well as for the general population.
2) “They think they’re contagious once diagnosed.” Dr. Young says patients often worry that they will transfer this cancer to other people- which is absolutely not true.
- How do you approach conversations with patients about the role of HPV in their diagnosis and the importance of HPV vaccination?
Dr. Young explains that he starts by clarifying that: “The virus was there a long time ago, and it’s most likely gone, it just layed down some genetic framework, and for whatever reason, we don’t know, 20, 30, 40, even 50 years later, got triggered again and is causing a tumor to grow”. Dr. Young takes the time to explain to patients in layman’s terms the biology of how their disease came about.
Next, he’ll explain “Patients always ask me what can I do?, what can we do?, and that’s when I say the most important thing we can do is make sure that people understand that this is a potentially preventable disease and if we can get vaccination rates high in this country, we may be able to eliminate this cancer altogether.” If asked for evidence of this framework, Dr. Young will frequently cite what Australia has managed to accomplish, they’re cervical cancer and RRP rates have dramatically decreased, rarely seeing new cases in vaccinated mothers, “and that’s a country with a 95% vaccination rate. This is not theoretical, we have science here.”
- Are there specific signs or symptoms of HPV-related head and neck cancers that people should be more aware of?
Dr. Young states that patients often say I had no idea until I felt this lump in my neck– so he reminds patients that they did the right thing by seeking care, “if there is a neck mass, that hasn’t been there before, that persists for more than 30 days, they should probably have it checked out. A neck mass in an adult is likely something that needs to be assessed or biopsied.”
Dr. Young also says to be aware of “changes in ability to swallow, change in voice, difficulty swallowing, painful swallowing, coughing up blood or things or that nature should trigger an instant trip to an ENT (Ear, Nose, and Throat) doctor.”
“The majority of patients with this disease (oropharyngeal cancer) present with a neck mass.” Dr. Young’s personal take is that “these tumors are related to a virus biology that produces warts… It produces tumors that tend to grow out of things rather than into things.” Dr. Young proposes this is why many patients are asymptomatic in the throat until it becomes a size that interferes with functionality, such as swallowing or talking.
- What are the biggest gaps in care that still need to be addressed for HPV-related cancers?
Dr. Young begins his response by acknowledging how lucky we have been with cervical cancer screening (the Pap Smear), but unfortunately there is no such screening tool for oropharyngeal cancer.
“It is meticulous – making sure you schedule your general health care. Make sure you’re seen once a year by your family physician. If you palpate (feel) something on your neck that wasn’t there before, have it looked at”. He also notes, regarding non-hpv related head and neck cancer, attending annual dental exams are important as a form of cancer screening.
It boils down to normal preventative care. Dr. Young makes a point to mention that the COVID-19 pandemic taught us “that there were a lot of delayed diagnoses of cancer during that time of isolation, and if we ever have another pandemic where access to healthcare is limited, we’re going to have to come up with better ways to screen people at home. This could follow the lines of cologuard, blood-borne online platforms, AI, and telehealth that could supplement healthcare populational limited access to healthcare. Those tasks are on the watchlist for the medical community as a whole.”
Recurrent Respiratory Papillomatosis (RRP)
- You’ve been involved with RRP awareness—what are some of the biggest challenges in treating this condition?
Dr. Young is a dedicated advocate for Recurrent Respiratory Papillomatosis (RRP), board member of the RRP Foundation, and father to a son diagnosed with Juvenile-Onset Recurrent Respiratory Papillomatosis (JORRP). “Regarding RRP, we have some educational gaps”. Dr. Young says that experts go straight to surgery for treatment to keep the airway open, but from a patients’ point of view, that’s the worst outcome. Dr. Young says that patients and families want non-surgical options.
This disease means tumors driven by HPV, we need HPV-tumor targeted therapies, Dr. Young says. “We should be eliminating the need for surgery by providing alternatives”. Dr. Young also mentions that “physicians are not often presented with cases of RRP, so seeking out specialized care is important. This may be challenging in rural areas, but just seeking the opinion of a physician with experience in RRP can be huge.”
- What do you wish more people, including healthcare providers, understood about the impact of RRP on patients and families?
Dr. Young emphasizes the profound impact of recurrent respiratory papillomatosis (RRP), stating, “I think that it’s really important to understand that this disease (RRP) is a devastating diagnosis for most individuals.” Patients and their families often endure immense emotional and logistical challenges, navigating complex treatment options and traveling to specialized centers- this is an overwhelming burden that can take a significant toll.
Beyond the physical and emotional strain, the stigma associated with an HPV-related disease adds another layer of hardship. Dr. Young notes that many mothers he encounters struggle deeply with feelings of guilt, fearing they may be responsible for their child’s diagnosis.
However, he remains hopeful about the future of treatment. “This is where we can use the biology of the virus to our advantage,” he explains, emphasizing the potential of ongoing research into alternative therapies that build upon our existing understanding of HPV.
Key Takeaways from Dr. Geoffrey Young
- What advice would you give to patients and caregivers navigating an HPV-related cancer diagnosis?
1) “First, know that 95% of oropharyngeal cancers present at a treatable stage, which means there are many effective treatment options available.”
2) Dr. Young strongly encourages patients to consult with specialists across different fields such as medical oncologists, radiation oncologists, and head & neck surgeons to ensure they receive the most comprehensive and personalized care. “Seeking treatment at a center with expertise in head & neck cancers or RRP can make a significant difference in outcomes and quality of care.”
3) “Remember that you are not alone.” There are numerous resources and support networks available to guide and empower both patients and caregivers. Organizations like the Head & Neck Cancer Alliance, HPV Cancers Alliance, and dedicated patient support groups offer education, community, and advocacy to help you navigate this journey with confidence.