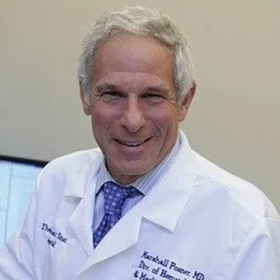
In the Office with Dr. Marshall Posner
Dr. Posner is a Professor of Medicine at the Icahn School of Medicine at Mount Sinai, NY. He is the Medical Director of the Head and Neck Oncology Program, Associate Director of the Center for Personalized Cancer Therapeutics, and co-Director of the Cancer Clinical Investigation Program for the Mount Sinai NCI – National Cancer Institute-designated Cancer Center.
Is head and neck cancer on the rise and why?
Yes, head and neck cancer caused by HPV has been rising substantially and continuously since it was first identified in 2000. If we look back over the 20 years before that and we have tissues and blood tests to examine, we can see that HPV positive cancers began to increase several decades before 2020, and they have continued to increase such that the incidence has increased dramatically. In fact, 75% of the cases we see at Mount Sinai are HPV-positive oropharynx cancer. On the other hand, we have also seen a large reduction in drinking and smoking-related cancers. I think this reflects changes in our society including a great awareness of tobacco as a carcinogen and tobacco being very dangerous and harmful to people’s health as well as highly addictive.
If we look back at the causes for the rise of HPV, I think you can look at them as a socio-infectious disease process involving the mixing of the different populations within the country, people from rural areas moving into cities and back, for example. In rural areas, there’s great separation, less density, and reduced impact of people being close together and having a lot of relationships compared to the cities where people are densely packed. Also, the changes in the sexual mores and the way people really connect with one another have altered the risk. I think that we’ve seen an amazing increase in the rate of HPV infection and the frequency of sexual contact. I think that is clearly related to the transmission of the disease because it is an infectious virus that causes this. That being said, the rate is still relatively low, but it’s increasing, and we expect to see something on the order of 30,000 cases next year. Also, different sites within the head and neck appear to be involved as we have become better at detecting the virus. Not only is the base of the tongue and the tonsil – the oropharynx a major site, we’re also seeing about half of the nasal cavity cancers being caused by HPV as well. And one can argue that that’s a hard place to get to sexually, but it is a place where you can auto transmit. And so you’re seeing an increase to about 50% of sinus cancers being related to HPV.
How does HPV cancer spread in the body? Are you suggesting that an HPV infection can move from one area of the body to another?
Yes, I am assuming that people touch their sexual organs and they touch themselves in the mouth and put their fingers in their nose. It’s important to know that HPV has to spread by transmission of bodily fluid like saliva or semen, or vaginal or anal secretions directly to a mucosal membrane. It is not spread through blood exposure.
If someone knows they have high-risk HPV, what would you recommend they do to get screened. Should everyone be screened for head and neck cancer the way all women are screened for cervical cancer?
Well, right now there is no good screening process for head and neck cancers. The cervix, the vagina, the anus, are all relatively limited areas and be examined easily if not comfortably. These are very localized areas. But not the oropharynx. If you spread out all the mucosal tissues of the oropharynx, it would be a big piece of skin or mucous membrane and it’s all full of ridges and little canyons where things can hide. Furthermore, it is physically difficult on the patient to examine this area closely because of the gag reflex and breathing control. So, it would be virtually impossible to physically visualize the whole oropharynx. Secondarily, the tumors in the oropharynx can spread to lymph nodes in the neck nodes and burn out in the original site in the oropharynx. They can also be submucosal, which is underneath the surface. So, you may not see them even if they could become quite large with a visualization. There is no good PAP smear you can perform here. There is now a saliva test that is utilized in research to look for HPV high-risk types, but we don’t know the precise relationship of positivity with this test to the development of oropharynx cancer.
We do know the antibodies to high-risk HPV proteins appear in the circulation up to 10 years before cancer appears, and that they’re highly related but these are not an approved test and remain a research tool at the moment.
So we really don’t have a good screening tool. The best screening tool is for people to be alert and if they develop a persistent sore throat, if they have a neck node, if they have difficulty swallowing or changes in their voice they should see an ENT. Those are signs of cancer.
There is a new test. It’s being developed; it is a blood test for cell-free HPV-DNA. As I said, the virus doesn’t circulate in the bloodstream, but when one has cancer, and when the cancer cells die, there are DNA products from the virus that gets into the circulation. If you have an active cancer, you can measure fragments in the blood. This test could be used as a screening tool, as well as a prognostic and predictive tool. So now when we get a patient who has a lump in the neck, or a lump in the throat, even though it’s not an approved test, we will also get a cell-free HPV-DNA and confirm the diagnosis. This is not a sensitive tool. Antibodies are probably more sensitive. We don’t’ know the rate of false positivity for the antibodies. I don’t think you can have a false positive cell-free HPV-DNA test unless you’re having a transient infection. I don’t believe that transient or low-grade infection has been looked at closely. This would be particularly important in anal cancer where there are a lot of low-grade lesions that are HPV positive and regress. Determining which ones are going to progress to cancer is one of the issues and how to treat that is a big question. We don’t’ have that luxury here of a regressing lesion we can observe in the oropharynx.
There are HPV cancer screening studies going on now. We are part of a federally funded one and collaborate with Johns Hopkins and other institutions on this trial. When HPV cancer patients come to us, if they have a family member, or if a subject has a pre-existing condition that might put them at risk like HIV or if they have a history of cervical dysplasia, we will screen on them in this study. The study is designed to examine 4000 people in the high-risk categories. We test saliva, urine, vaginal secretion, and blood for HPV and perform a physical exam.
When a patient screens positive, then we have added more traditional screening tests: radiographic screening tests and a further physical evaluation. We see those patients who have screened positive in follow-up regularly if they don’t have an identifiable cancer.
I know a lot of survivors of HPV cancers who worry about getting another HPV cancer in a different part of the body. What are your thoughts about that and how can such people be screened?
It is possible that they will get a second HPV cancer although it’s rare, and I’ve had patients who had oropharyngeal cancer who developed vulvar cancer and a patient with anal cancer who developed a tonsillar carcinoma and whose spouse developed a tonsillar carcinoma. It is rare enough that I remember them. So it is possible to see low level second and partner cancers. It’s not very common, though, and the risk is quite low. But if you want to do screening as a former patient, I think the best screening is not going to be an antibody because those are long-lasting and will not disappear when cancer disappears. But to do the cell-free HPV-DNA is a reasonable screening test. Unfortunately, it is not validated or approved, so it’s really my opinion and not an official recommendation.
That being said, If I had a history of cell-free HPV-DNA in my blood, I would want to get tested and evaluated on a regular basis. And there are several groups that have developed the technology and have been approved for use in patients. There is a commercial entity that has it. I have to reveal that I have advised them in the past, but they have a commercial one. We have also developed a test here at Mt Sinai and will have the test validated shortly for use in patients. In the meantime, we use a commercial test. Finally, I would recommend that if you’re concerned then the HPV vaccine is available for use in people up to the age of 45. If you are over 45, this becomes a personal decision. The vaccine is very safe, and I would not have qualms about using it myself if I were worried and over 45.
Finally, If you screened positive by a cell-free HPV-DNA, and no tumor was identified, you could consider getting into a trial for that population. Currently, there is no available trial that I am aware of but I am sure that one will be available in the future.
You’re suggesting that the Gardasil vaccine in people who already have high-risk HPV can reduce second HPV cancers?
I’m suggesting that if your partner has it, or you have a history of having been infected such as HPV positive cervical dysplasia there is evidence that it might prevent the development of cancer.
If you had a positive PAP smear and you are under 45, once you clear that PAP smear, you should consider getting the vaccine.
How are head and neck cancers treated and what are recent developments in treatment?
Right now the principal treatments are surgery, chemotherapy, and radiation. These are the three arms of multidisciplinary care in head and neck cancer. Treatment can be a single modality for surgery and radiation or a combined treatment using 2 or 3 treatments. Chemotherapy is currently not curative by itself and SIRS as a booster to the other treatments.
The tragedy and the scandal of oropharyngeal HPV cancers is that there has been no movement to reduce the standard care beyond the very intensive treatments that are available While there have been multiple studies, almost none of them have been what are called phase three trials that have actually moved the needle in terms of treatment. The trials have not been aimed at definitively reducing radiotherapy which is the major cause of short and long-term toxicity for patients This is a huge scandal that has been perpetrated by the NCI and the leadership of the cancer clinical trials networks at the behest of the radiation oncology community. Unfortunately, there has not been a single definitive dose reduction phase 3 trial aimed at reducing radiation treatment activated or completed in this country while there have been multiple trials that have been called “dose reduction” most of them in phase two. Many were not truly productive trials as they reduced chemotherapy by switching from cisplatin to a different type of chemotherapy and were predictable results; they showed that we cannot eliminate or switch this highly effective drug. This is a huge scientific failure on the part of the leadership and it is a moral failure on their part for not effectively addressing the major toxicity of treatment of head and neck cancer and particularly HPV-related oropharynx cancer which is radiation therapy.
And you know I would call them out on this any time they would have a notion to ask me and others to give an honest appraisal of the results of their trials and listen to us. I have put this forward in multiple conversations. I and many other investigators have full research programs in de-escalation of treatment for patients with HPV; however, none of these are Phase 3 trials. Phase 3 trials require enormous resources and federal funding. No pharmaceutical company will support this work as it will not lead to product approval. This is completely a failure on the part of the cooperative groups. Many individuals within the cooperative groups want to have Phase 3 reduced dose treatment studies. They just simply cannot get approval from the NCI leadership and this is a significant problem.
So people are getting too much radiation and getting too many side effects?
They are getting too much. Both short and long terms side effects; scarring, fibrosis, stomach tube dependence, dental failure, vascular lesions in the carotids which will develop in these patients over decades, thyroid failure, which is easily treatable, and on and on are related to radiation therapy dose.
A small and real fraction of people also get second cancers if they survive long enough, from high doses of radiation. In one of our studies, we did a small randomized trial of standard-dose chemoradiation therapy in non-smokers versus reduced-dose radiation with chemotherapy for patients. One of our control patients developed a second cancer right in the middle of the radiation field. The tumor was P53 positive, HPV negative, and P16 positive. It was easily treatable for this man because he was under surveillance. But this was seven years after he had his radiation, so this may prove to be a significant problem.
And current treatment is bound by the existing protocols when you treat patients even though you would prefer to give patients less radiation, right?
If a patient comes and says “I don’t want to be in a trial, I just want the reduced dose” then we cannot give this patient this treatment except under a trial. It’s not an approved therapy. If that patient were to relapse, they could rightly turn around and say “you didn’t give me the proper treatment.” We can’t provide a reduced dose treatment as part of SOC without the results of randomized clinical trials demonstrating it was a safe and effective treatment.
So, you are advocating for such trials?
I am stamping my feet and screaming loudly for these trials.
What do you recommend that people who are newly diagnosed with head and neck cancer look for in terms of their treatment?
They should look for an organization that is doing research and HPV clinical research and is advocating for real de-escalation and reduced dose treatment just as we are. They should look for a multi-disciplinary program. This should not be treated by radiation doctors alone, by a surgeon alone, or by a medical oncologist alone. This requires a coordinated and cooperative plan of therapy. They need to see a radiation oncologist, a medical oncologist, and a surgeon to weigh in on the individual patient’s risk factors that are unique to that patient and on the results and potential of the treatment.
That is the key. You are not going to find that at most community hospitals and the community doctors are bound by the standard of care to give standard-dose chemotherapy and radiation. So, you’re not going to get the opportunity to participate in a de-escalation trial without going to a cancer center that has research in these trials or is participating in a randomized national cooperative trial.
Is there anything else you want to tell people in general what should people know?
People should know this is curable. It’s highly curable and what they really need is to get the proper therapy for their risk level and that that is probably the best thing that they can do
There are ways to prevent getting cancer. If you are highly promiscuous where this is an addiction that you cannot control and not an act of empathy, then you should get some help because acting out will put you at higher risk. There is a higher risk if one has many sexual partners. I also personally believe, without data, that HPV is transmitted by intimate kissing. We cannot escape intimate relationships. Having intimate relationships is necessary; we grew up in packs and need people around us even though we aren’t living in small groups anymore. Humans need social communication; isolation leads to significant destructive emotional issues. We need empathy, we need relationships, we need physical relationships, so we shouldn’t deny that, but we should weigh the health risks. When HIV first came out, it was transmitted sexually, and you would see people with hundreds of contacts a year as the most vulnerable population getting it. HPV is a different disease, it’s not 100% penetrant, it’s a lot less risky, but you really are upping the game if you are in a highly promiscuous setting. And I’m not making a judgment; I’m just laying out the facts. About 20% of HPV cancer is related to promiscuity.
You are just stating the fact that the more sexual partners someone has, the more risk they have of contract high-risk HPV?
That’s oral sexual risks as well as vaginal sexual partners in general. Mouth-to-mouth kissing may also transmit (not a kiss on the cheek, but with an exchange of saliva). This is an exchange of bodily fluids and we know that some forms of HPV lives in the oral cavity intermittently and that people have non-high-risk HPV variants in their oral cavity, and about 3% of people without having cancer will have a high-risk variant like HPV 16 detectable in their saliva at any one time. Salivary high-risk HPV may come and go in many people.
Are HPV head and neck cancers caused by HPV 16 or by other strains?
They are mostly caused by HPV 16. About 15% are caused by other strains, and there are very particular strains that cause it as opposed to ones that cause cervical cancer. The biology of oropharynx cancer and anal cancer is quite different than cervical cancer and nasal sinus cancer. Sinus cancer is a lot more like cervical cancer than it is like oropharyngeal cancer.
Sinus cancer is not that common a tumor, so we don’t have enough experience with this population to know if testing patients with sinus cancer for cell-free HPV DNA may be helpful or the relative prognosis. Also, about half of sinus cancers are not HPV-caused.
What should we be advocating for more?
We should be advocating for early vaccination. It’s a totally preventable disease. We should urge men and women until the age of 45 to be vaccinated and particularly if you have an intimate contact who has HPV or has had HPV cancer, I recommend vaccination at whatever age, frankly. Even though there is no documentation that the vaccine is preventative over the age of 45, I’d venture to say it is quite likely to affect people over the age of 45 as well.
Anything else anyone should know?
Frankly, I would travel 200 miles a day to get reduced-dose radiation. That’s how significant a problem it is. If I were anywhere within 200 miles of this location, I would do it. I would not want the agony I see in my patients when they get the standard dose. It’s devastating. It’s traumatizing.